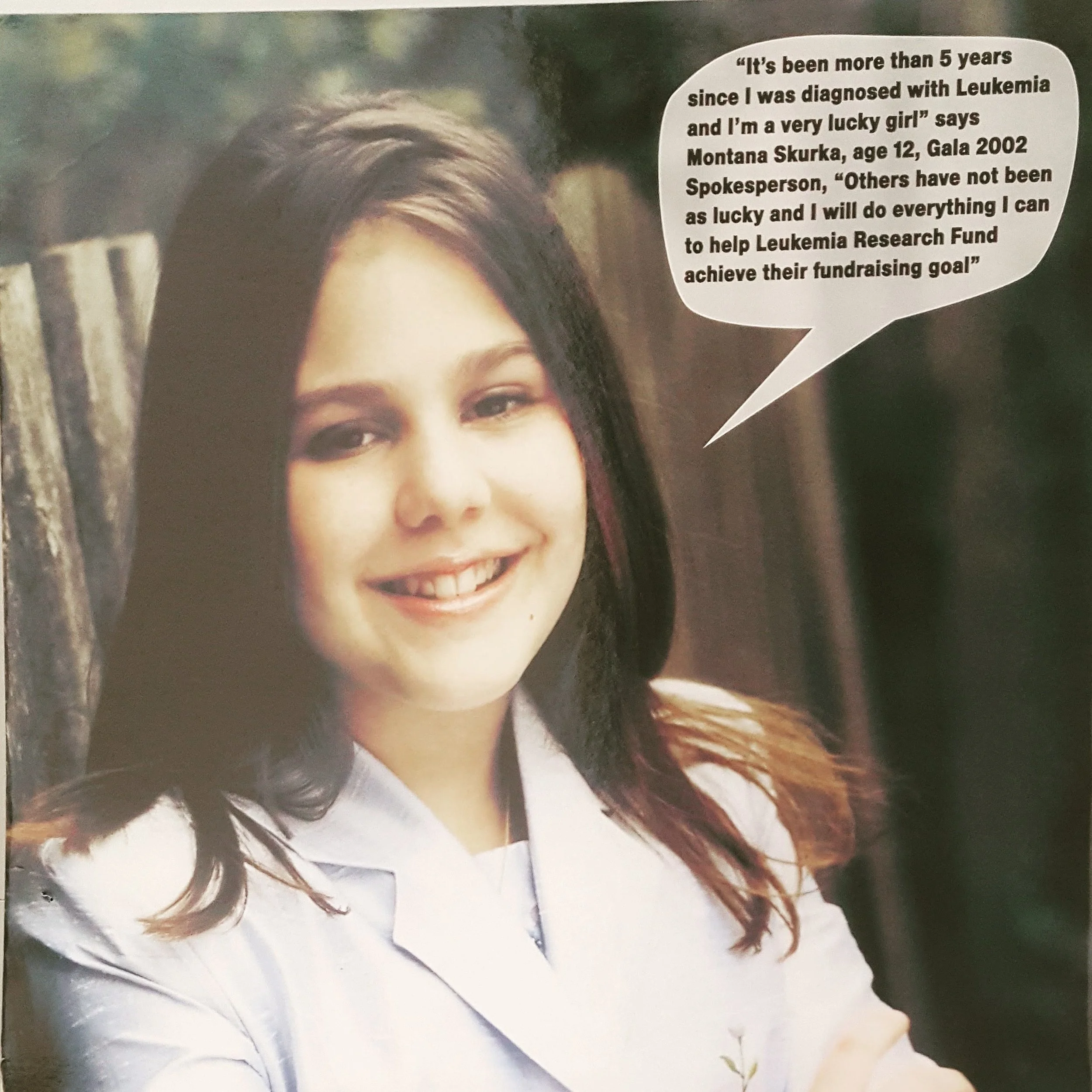
Hi, I’m Montana ⋆˙⟡
I’m an Integrative Therapeutic Practitioner, Speaker and Educator.
I support people who live inside bodies shaped by illness, chronic stress, pain and uncertainty. I also work with healthcare teams who are navigating the emotional, relational, and nervous system demands of caring for others.
Many people look “fine” on the outside, but inside they are living with fear, vigilance, disconnection or exhaustion. They are managing symptoms, but they don’t feel at home in themselves.
I know this experience personally and professionally.
I was treated for childhood cancer at the age of seven. As a teenager, I was diagnosed with Inflammatory Bowel Disease. Much of my life from a young age up to my twenties was shaped by being a patient, living in medical systems and experiencing the distress of a body holding onto experiences long after a crisis has passed.
What I needed then was not more advice or information.
I needed help finding safety within my body to build trust with my life and hope for the future.
That is the work I do now.
My approach
My work sits at the intersection of lived experience, clinical understanding and embodied practice.
I help people understand why their nervous system responds the way it does and how to work with that response rather than against it. Through mindfulness, therapeutic movement, sound meditation, education, and creative reflection, I support people in building steadiness, choice, and inner capacity.
This work is not about fixing or forcing change.
It is about learning how to stay present with what is real.
It is about widening the space between trigger and reaction.
It is about finding a way to move forward with more clarity and self-trust, even when health or life remains complex.
For Healthcare Providers
I have spent the past decade designing and facilitating programs, workshops and talks across healthcare, academic and community settings.
My background includes:
Leading national patient education and support initiatives with Crohn’s and Colitis Canada
Facilitating mindfulness, yoga, and group programs for patients, caregivers and staff at SickKids Hospital
Speaking at conferences, hospital rounds and professional education events on chronic illness, mental health, and embodied coping
Collaborating with interdisciplinary teams across medical, mental health and wellness contexts
My work with healthcare professionals focuses on two equally important areas:
Supporting clinicians in understanding the lived, nervous system experience of illness, so patient care can be more attuned, compassionate and sustainable.
Supporting clinicians themselves. Healthcare work is inherently demanding. Repeated exposure to suffering, high responsibility, moral distress, and systemic pressure takes a real toll on the body and mind.
I offer practical, experiential tools that support self-regulation, resilience, and reconnection, both individually and within teams. This work often helps professionals:
Recognize their own stress responses without judgment
Prevent burnout through nervous-system-aware practices
Feel more resourced and present in clinical interactions
Reconnect with meaning in their work
My role is not to replace clinical care, but to complement it by addressing the human and embodied dimensions that shape both patient outcomes and provider wellbeing.
Let’s connect
This work is for anyone who feels disconnected from themselves after illness, prolonged stress, or difficult life experiences.
You do not need a diagnosis to belong here.
You do not need to identify as a “patient.”
You do not need to be in crisis.If you are looking for a grounded, honest way to reconnect with your body and your life, you are in the right place.
My intention is simple:
To help people move out of survival mode and into a more connected relationship with themselves
To support identity shifts beyond the passive patient role
To create spaces where growth & transformation naturally emergesBecause we cannot separate the body from the mind, nor do we heal in a straight line.
Rather, healing is a deeply human and nonlinear process that must include all aspects of our humanity: our emotions, relationships and identity.
If you’d like to collaborate, book a talk or explore working together, I’d love to hear from you.